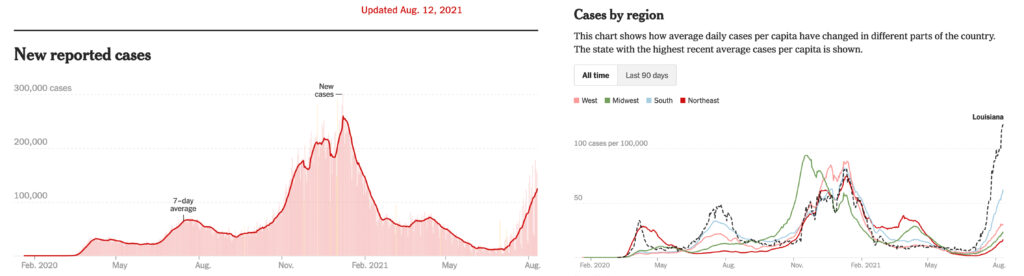
COVID-19 infections and hospitalizations are increasing rapidly in the United States as the highly contagious delta variant of the virus spreads. The situation is particularly dire in the South, where hospital intensive care units in many areas are nearing or reaching capacity.
The delta variant, which can make people sicker than the original virus strain did and is causing serious illness in younger people, can be contracted during “fleeting contact” of less than a minute.
To learn more, see the questions and answers below, along with links to relevant studies.
1. What is the delta variant?
Delta is a highly contagious strain of COVID-19. It was first identified in India in December of 2020. It swept rapidly through that country and Great Britain and has now spread to more than 100 countries.
Delta has quickly become the dominant COVID-19 strain in the United States. The Centers for Disease Control and Prevention reported in early August that the delta variant accounted for 93% of U.S. cases. In May, it accounted for only 3% of cases.
2. How is delta different from other variants that we’ve seen so far?
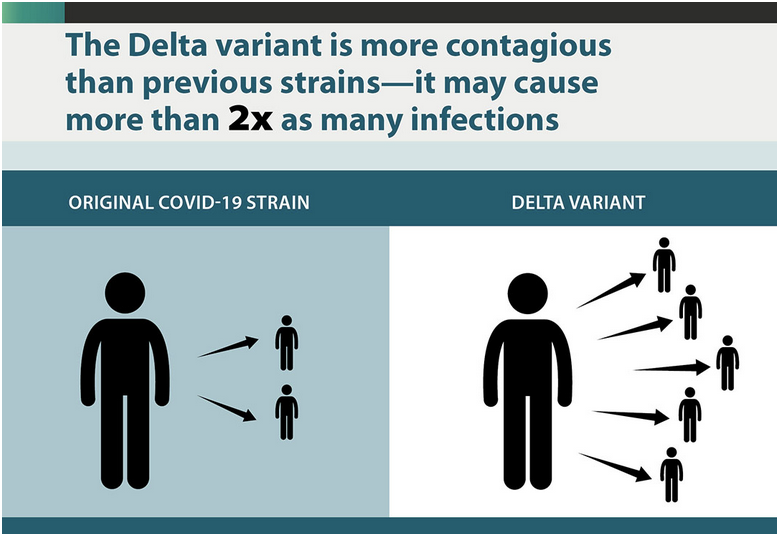
Delta is 60% more contagious than the Alpha strain, which was 50% more contagious than the original strain of COVID-19. This makes it twice as transmissible as the original COVID-19 strain. People who are infected with delta have—on average—about 1,000 times more copies of the virus in their respiratory tracts than those infected with the original strain and are infectious earlier in the course of their illness.
A recent study from the United Kingdom showed that children and adults under 50 are 2.5 times more likely to become infected with delta.
3. Does the delta variant make people sicker than the original COVID-19 strain did?
In two different studies from Canada and Scotland, patients infected with the delta variant were more likely to be hospitalized than patients infected with Alpha or the original virus strains.
4. How is it spread?
The primary way the virus spreads remains being indoors with someone who is infected and breathing in their droplets or aerosols. With delta, the difference is that the infected person will make many more copies of the virus and make them faster, causing the virus to spread more easily.
5. What are “aerosols” in relation to COVID-19?
Aerosols are infectious viral particles that can float or drift around in the air. Aerosols are emitted by a person infected with coronavirus — even one with no symptoms — when they talk, breathe, cough, or sneeze. Another person can breathe in these aerosols and become infected with the virus. Aerosolized coronavirus can remain in the air for up to three hours. A mask can help prevent that spread.
6. How long do you have to be near someone with delta to catch it?
Less than a minute. Contracting the original strain of COVID-19 took 15 minutes of prolonged contact with someone who had the virus. Health officials are warning that transmission of the delta virus can take less than a minute. There are documented cases of it happening with only “fleeting contact” of 5 to 10 seconds between unmasked individuals.
7. What are the most common symptoms of the delta variant?
Headache, sore throat, runny nose, and fever are the most frequent symptoms. Cough and loss of smell are reportedly less common with this strain.
8. What are the potential long-term effects of COVID-19 infection?
According to the CDC, the most common lasting symptoms are fatigue, shortness of breath, cough, joint pain, and chest pain. Other issues include cognitive problems, difficulty concentrating, depression, muscle pain, headache, rapid heartbeat and intermittent fever. It also can cause lasting damage to the lungs, heart, nervous system, kidneys, liver, and other organs.
Long-term COVID-19 is showing up in children as fatigue, depression, shortness of breath, heart inflammation, damage to the heart, and other long-hauler symptoms. Heart inflammation is particularly concerning in young athletes returning to their sports after mild or even asymptomatic COVID cases.
A mysterious form of diabetes and dementia-like symptoms that could indicate an elevated risk for Alzheimer’s disease have also resulted from COVID-19 infections and are being studied.
9. What prevention measures are doctors and public health experts recommending?
Since people who have not been fully vaccinated against COVID-19 are most at risk for serious illness and death, doctors say the most important thing you can do to protect yourself from delta is to get fully vaccinated.
Following CDC guidelines for vaccinated and unvaccinated individuals also can help you protect yourself and others. Because evidence is now clear that a significant portion of vaccinated people can become infected with the delta variant and pass it to others, the CDC changed its guidelines for vaccinated individuals on July 27. (Vaccinated people are very unlikely to become seriously ill or die from the delta variant; more on that below.)
The CDC now recommends that everyone, even those who are vaccinated, wear a mask indoors if they live in an area with high or substantial transmission rates, according to the map below. Currently, this means people in the vast majority of the United States. Health experts are also calling for the use of high-quality masks, such as N95 masks, because they are better than cloth or surgical masks at reducing the spread of infectious coronavirus particles.
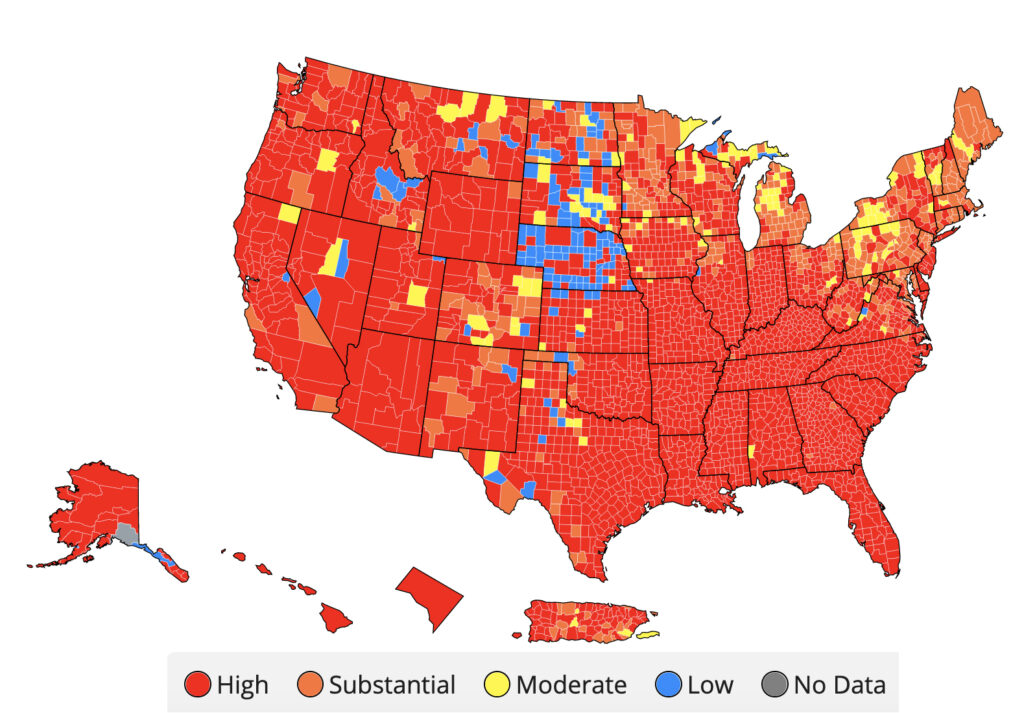
Health experts also recommend keeping six feet of distance between yourself and others (although transmission can occur at distances greater than six feet; particles from an infected person can move throughout an entire room or indoor space) and avoiding indoor spaces with crowds or with inadequate ventilation with outdoor air. They also recommend taking into account the vaccination and case rates in your area.
10. How effective are vaccines against the delta variant?
The delta variant is more likely than other forms of the virus to cause infections in people who have been vaccinated, and vaccinated people who become infected with this variant are more likely to spread it to others.
Though it’s still possible to get infected by the delta variant while fully vaccinated, the vaccines dramatically reduce the risk of serious illness or death. Multiple studies show vaccines are highly effective at preventing serious illness and death.
A Public Health England analysis showed the Pfizer-BioNTech vaccine was 88% effective against symptomatic disease and 96% effective against hospitalization from delta. Recent data from Israel’s health ministry showed the Pfizer vaccine was 92% effective against hospitalization and 91% effective against severe illness caused by the delta variant. In a study from Ontario, Canada, researchers estimated the effectiveness of the Pfizer/BioNTech vaccine against symptomatic infection with delta to be 87% after two doses. Moderna has reported on studies (not yet peer-reviewed) that showed only a modest reduction in effectiveness against delta compared to effectiveness against the original virus. Johnson & Johnson also has reported that its vaccine is effective against delta, but one recent study, which has not yet been peer-reviewed or published in a scientific journal, suggests that the J&J vaccine is less effective against the variant compared to the original virus.
11. Can vaccinated people get long-haul COVID?
While the risk of getting sick if you’re vaccinated is very low, it’s still possible to end up with long-haul COVID-19 symptoms.
12. How bad is the current COVID-19 surge in the United States?
Infections and hospitalizations are increasing rapidly as the delta variant spreads. For the first time since February, the United States is averaging more than 100,000 new cases a day.
The outlook is especially dire in the South. Records for seven-day case rates were recently set in Florida and Louisiana. Hospitalizations in Florida are equal to their previous peak from last summer, and in Louisiana, intensive care units are strained.
13. What is the outlook for the future?
Human behavior is likely to be the most important factor in the pandemic’s course. MIT Medical Director Cecilia Stuopis states: “We don’t need to panic, but we do need to take personal responsibility for doing what’s necessary to protect ourselves, our families, and our communities. Right now, it’s delta. In the fall it may be kappa or some other, fitter variant. We can’t be complacent. We are going to be living with this virus in some form or another for the foreseeable future, but our actions right now can determine what that future will be.”